NOW REPORTING FROM BALTIMORE. An eclectic, iconoclastic, independent, private, non-commercial blog begun in 2010 in support of the federal Meaningful Use REC initiative, and Health IT and Heathcare improvement more broadly. Moving now toward important broader STEM and societal/ethics topics. Formerly known as "The REC Blog." Best viewed with Safari, FireFox, or Chrome. NOTES, the Adobe Flash plugin is no longer supported. Comments are moderated, thanks to trolls.
Search the KHIT Blog
Thursday, December 26, 2013
Holiday respite
Been a very busy year, as will be 2014, no doubt. But, I'm taking a hiatus of 11 days just eating, sleeping, reading, and thinking while I enjoy family time.
Hope you are are doing the same, and have a great year ahead.
___
More to come, as always...
Wednesday, December 18, 2013
ICD-10: W6142XA, Struck by turkey, initial encounter
Loves me Adobe Suite Photoshop.
From today's post on THCB: Does ICD-10 Pilot Forecast a Perfect Storm for Healthcare?
...The ICD was a tool designed by epidemiologists to get some handle on the prevalence of disease. It was always a blunt instrument, suffering from lack of reliability and of validity of the categories, a lack that was both temporal and geographic. Why anyone could ever imagine that such soft categorizations could be harnessed to capture more than the crudest measure of the experience of illness is baffling. And anyone who imagines that most illness experiences can be parsed into reliable and valid components is deluded into thinking that “health care” can be managed with the same tools that make Sam’s Club and Costco so successful. Stocking cans of vegetables is as concrete as illness narratives are abstract. All we will do trying to codify illness into its components is create cadres of coders and auditors, administrators and regulators, data generators and analyzers, and … so many that we’d be better off letting the inmates run the asylum...I'm reading Dr. Hadler's latest book The Citizen Patient and will be reviewing it shortly.
The ACA has much that is noble in intent and much that deserves celebration, not the least of which is universal access regardless of prior illness. But treating health care as a “free market” is delusional: There is no caveat emptor since the patient is insured for much that is unnecessary and is blamed for poor outcomes: If the can of vegetables is spoiled, Costco will replace it, apologize and take the issue up with its supplier. Try that in the US medical system. You’ll end up in a tort.
Unfortunately, I see no way to head off the impending chaos. I see escalating expense, blame and culpability, lay-offs and bankruptcies, all as the price of the billing scheme that drives the implementation of the ACA, a billing scheme that pivots on ICD-10.
There are other approaches that are far more rational and that take the patient and the patient’s experience of illness as the primary raison d’être:
For example:
Maybe such will be the Phoenix.
-Norton M. Hadler, MD
apropos, some context from Dr. Hadler regarding medical coding.
By 1970 all the pieces and players were assembled for the American health-care system to become more a cash cow (Figure 3) than a service profession. It has today become a herd of cash cows, particularly in the United States (Figure 4). The seeds of the trend were in the “reasonable cost” clause of the Medicare legislation. No longer was a sliding scale of fees-for-services supporting a cottage industry. The government and large employers were the de facto consumers of services. The compromise with the AMA to permit “usual and customary” fee-for-service charges is embodied today in yet another new age industry dedicated to defining “service” and setting “fee.” In 1966 the AMA first published Current Procedural Terminology (CPT), a set of codes designed to standardize billing for “Evaluation/ Management Services” (E/ M). The CPT Editorial Panel currently meets three times a year and releases new editions each October to reflect changes in practice. The current version lists numerical codes for more than 10,000 procedures and services.There is no reproducible evidence that the EHR decreases medical errors or increases compliance with “standards” for quality of care. Rather, the purveyance and servicing of EHR has joined coding as yet another profitable industry."
CPT is the most widely utilized medical nomenclature in reports to public and private health-insurance programs in the United States. In 1983 it was mandated for all billing under Medicare and Medicaid. CPT is also a profitable proprietary undertaking for the AMA, which sells all sorts of educational and other aids to assist in the coding exercise. After all, hospitals and physicians need to be able to accurately code for E/ M services or they risk loss of income or fraudulent billing accusations. “Coding” is a burgeoning job category that appeals to many, even to many in the nursing profession. There are courses offered in coding in all sorts of venues, including many junior colleges. Coders are checking on coders, and physicians are admonished if they do not “document” in their records for the sake of coding; they are less likely to be admonished if the content of the record communicates poorly about actual patient care. In fact, coding and billing are driving the design of the Electronic Health Record (EHR) in America. There is no reproducible evidence that the EHR decreases medical errors or increases compliance with “standards” for quality of care. Rather, the purveyance and servicing of EHR has joined coding as yet another profitable industry.
Although the costliness of health care had yet to take off (Figure 4), the inefficiency of paying usual-and-customary fees for each and every coded item was obvious early on, particularly for Medicare and Medicaid patients treated in hospital. It made more sense to pay a lump sum for a particular package of care, a “product” such as a total hysterectomy or an appendectomy. In the 1970s, the Health Care Finance Administration (HCFA), the predecessor agency to the CMS, contracted Robert Fetter, Ph.D., and John Thompson, Ph.D., of Yale’s School of Management and School of Public Health, respectively, to create a classification of such “products.” The result was 467 Disease-Related Groups (DRGs), the last of which was the “ungroupable” category. The intent was to replace cost-based hospital reimbursement with a prospective payment system based on a presumably homogeneous unit of care.
The system was tested in New Jersey between 1980 and 1983, after which it was adopted by the CMS. Many states have since passed legislation requiring the application of DRG-based billing to privately indemnified hospital care. As a prospective payment system, it was designed to provide incentives for efficient and standardized care. If the patient can be treated in hospital for a particular DRG at a cost less than the prospective payment, the hospital can keep the excess. But if the cost exceeds the allotment, the hospital eats it. Given the proliferation of procedures and the complexity of illnesses, the number of DRGs had escalated to 999 by 2007. Much of this relates to provisos for particularly complex or complicated “products.” By hook or by crook, coding was to make sure that the hospital continued to eat well enough to thrive. In 2008 the CMS declared that it would not cover all hospital-acquired conditions, particularly those deemed avoidable. This is a significant stride forward for competent care, since any degree of incompetence leads to codes that change the DRG in a direction that compromises the profitability of the not-for-profit hospital.
The DRG classification takes advantage of an internationally accepted system of disease classification that has its roots in the nineteenth century. The modern version is called the International Statistical Classification of Diseases and Related Health Problems (ICD), which is published by the World Health Organization (WHO) and widely used in the collection of mortality statistics and the like. The ninth edition, the ICD-9, allows for some 17,000 diagnostic categories and is used by the U.S. National Center for Health Statistics, which was instrumental in its development. The ICD-10 has been used since the mid-1990s— but not by the CMS, which adopted it only in the spring of 2013. ICD-10 is a classification system that allows for 155,000 different codes. One can well imagine how the proliferation of ICD codes will beget a proliferation of DRGs. The proliferation of codes is not simply a reflection of the proliferation of disease categories; some of the codes speak to the degree of severity and of complications. ICD-10 coding makes CPT coding look like child’s play. Hence, billing according to DRGs is a monumental task for all involved. Hospitals employ minions to find any nuance that might increase the complexity of the basic DRG in order to increase payment. The CMS outsources this billing to employ minions in the exercise of validating the charge package.
How much should any particular DRG cost? That brings us back to the “usual and customary” and “reasonable cost” roots. The hospital and hospital-supply industries are powerful and spared from most of the pressures of a true free market; they operate with a conspiratorial form of the “free market.” The same consumable or piece of equipment purchased from a laboratory supply house by an NIH-supported research laboratory can cost multiples more when purchased from a hospital supply house. The competition is set at a different level. The same is true for hospitals. Most hospitals will not publish their fee scale for room maintenance, nursing, and hospital services (such as X-rays or the running of operating rooms). Individual hospitals negotiate this fee schedule with individual private insurance companies. The hospital industry negotiates with the CMS, with provisions for the differences in cost in different geographic regions and with the help of lots of solicited and unsolicited “advice.” By law, hospitals must “accept” what the CMS pays even if it is less than their menu of prices for private insurers. Private insurance contracts have no such stipulation. Private insurers pass any bill in excess of the amount charged on to the patient. It’s a cozy arrangement that goes to great lengths to avoid transparency. There are even companies that help patients sort through their bills with the intent of finding overcharges that inflate co-pays. There is absolutely no doubt that this cozy arrangement is part of the explanation for the discrepant curves in Figure 4; the other part is overtreatment in the first place.
The best window into this cozy arrangement is the establishment of physician fees by the CMS. In the early 1990s, the CMS turned to the AMA for assistance with fine-tuning physician fees. This seems a logical extension of the role of the AMA in formulating CPTs. The AMA was to set aside “usual and customary” in favor of a new approach to a fair and accurate valuation of procedures and treatments by physicians. This approach was created by William Hsiao, professor of economics at the Harvard School of Public Health, and his multidisciplinary team of colleagues in the mid-1980s. They formulated and tested their Resource-Based Relative Value Scale (RBRVS) and submitted it to HCFA in 1988. In 1989 President George H. W. Bush signed the Omnibus Budget Reconciliation Act stipulating that the CMS base physician payments on the RBRVS. For every code in CPT, a fee was to be determined based nearly equally on physician experience and practice expense (recently, a dollop more was prorated for malpractice insurance). This is where the input of the AMA was sought. In 1991 the AMA established the Specialty Society RBRVS Update Committee (RUC) to advise the CMS as to the value of physician work and practice expense for the physicians providing any particular management/ evaluation service coded in CPT.
The RUC has twenty-nine members; twenty-three are appointees of major medical and surgical specialty professional societies and three are AMA appointees. All members sign confidentiality agreements before each meeting, which are closed to the public. The task is to calculate the Relative Value Units (RVU) for each CPT. Since the RUC is specialist dominated and heavily weighted to interventionalists, the RVU calculation is biased to value skills gained by lengthy training and the performance of tasks thought to be “stressful.” Cognitive specialties are given short shrift in this calculation. Furthermore, the process values effort over effect, which is contrary to the principles of evidence-based medicine. The incentive is to train to do more, even if the doing is ineffective. There is no incentive to be expert in informing medical decision making, particularly if the informing results in a patient’s desire to forego something with a high RVU. There is no incentive for higher quality performance or for caring for the more severely afflicted. RVUs are a perverse measure.
As is true of most areas of administration of the American health-care system, there is little transparency in the machinations that influence the CMS. That means there is little public debate. However, there is debate and controversy among the cognoscenti. The primary-care physicians who are not well represented on the RUC (except for the current AMA-appointed chair) and the cognitive specialists who are in the minority are crying foul. They want to be better valued. I am crying foul because this is an example of a public regulatory agency being controlled by the interests it is meant to regulate. The economists call this regulatory capture. I call it corrupt.
Hadler, M.D. Nortin M. (2013-04-01). Citizen Patient (H. Eugene and Lillian Youngs Lehman Series) (pp. 63-68). The University of North Carolina Press. Kindle Edition.
Well...We could relatively easily study the former assertion, but, doing so would not be cheap.
DECEMBER 19TH BREAKING NEWS
From: Sebelius, Kathleen (HHS/OS)That's pretty interesting. I certainly wish her well.
Sent: Thursday, December 19, 2013 11:19 AM
Subject: Important Staff Announcement
Colleagues,
I would like to announce that Dr. Karen DeSalvo, who currently serves as the City of New Orleans Health Commissioner and Senior Health Policy Advisor to Mayor Mitch Landrieu, will be the next National Coordinator for Health Information Technology here at the Department.
During her tenure, Dr. DeSalvo has been at the forefront of efforts to modernize the New Orleans health care system. Following Hurricane Katrina, for example, she led projects to increase access to care by augmenting the city’s neighborhood-based medical homes for low income, uninsured and other vulnerable populations in the New Orleans area.
Throughout her career, Dr. DeSalvo has advocated increasing the use of health information technology (HIT) to improve access to care, the quality of care, and overall population health outcomes –including efforts post-Katrina to redesign of the health system with HIT as a foundational element. She served as President of the Louisiana Health Care Quality Forum, the Louisiana lead for their health information exchange and regional extension center grants. She has also served as a member of the Steering Committee for the Crescent City Beacon Community grant.
As the New Orleans Health Commissioner she has made the increased utilization of HIT a cornerstone of the city’s primary care efforts and a key part of the city’s policy development, public health initiatives and emergency preparedness. Further, she has led the planning and construction of the city’s newest public hospital, which will have a fully-integrated HIT network. Her work as commissioner has led to positive changes to the way healthcare providers deliver care to their patients, improved accessibility and outcomes for patients, and improved the health of all New Orleanians. Dr. DeSalvo is a graduate of Suffolk University, Tulane Schools of Medicine and Public Health, Harvard School of Public Health.
Dr. DeSalvo’s hands-on experience with health delivery system reform and HIT and its potential to improve health care and public health will be invaluable assets to the Office of the National Coordinator and the Department. I would also like to take this opportunity to thank Dr. Jacob Reider, the Acting National Coordinator for his leadership of ONC during this time of transition. I am pleased she is joining our committed team, and ask you to join me in welcoming her to HHS when she starts on Monday, January 13th.
Sincerely,
Kathleen Sebelius
___
More to come...
Sunday, December 15, 2013
More #IHI25Forum
This was presented during one of the Keynotes. Really great.
Showed this to Cheryl yesterday. We've resolved to do more of what's recommended. We've both gotten too sedentary owing to our work ("Sitting is the new Smoking").
__
LEADERSHIP
Below: a personal focus of mine at IHI 25, notwithstanding my intense interest in so many of the enticing yet too-many-to-cover tech sessions:
In healthcare (albeit -- to be fair -- as is the case with enterprise more broadly), we love our totemic cliches. "Leadership" is too often one of them.
At my last place of employ we had a group of managers (HIT, HIE, and the ED) who summarily declared themselves "Leadership."
A noun. The Department of Leadership, I guess. The Ministry of Leadership.
They spent most of their time closeted away in lengthy hush-hush, FUD angst-incubating closed-doors meetings, emerging episodically to announce their latest summary edicts.
A particularly grating pronouncement to me was an emphatic and curt declaration one day by one of them during staff meeting: "now that Leadership has decided [regarding an as-yet truly operationally unresolved issue], discussion is over."
Okee-dokee. Irony-Free Zone, much?
This increasingly autocratic attitude was one factor in my decision to retire, quite frankly.
So, "Leadership." What of it?
Google it.
143 million results. While telling, too broad.
614,000 books. OK, now we're getting somewhere. What about Amazon?
107,615 hits just in the "books" category. My fiscally-enervating Whispernet 1-click strikes yet again, twice more.
I'd noticed these in the IHI 25 Forum bookstore. Snapped cover photos in my iPhone so I could review them on Amazon (the bookstore clerk was not amused). I've downloaded and just started them. (Uh, there's that equally dubiety-inducing word "Transforming").
MacCoby's work certainly looks intriguing.
So, persuasiveness cannot but be a core element of leadership, but what else?
I went to the day-long IHI pre-conference "Leadership Required for the New Era" for some timely and useful insights.
From their just-released White Paper:
Below, one of my favorite quotes, from way back during my time in IHC healthcare QI training.
I've never really thought of myself as a "leader." And I've never had any interest in its red-headed stepchild the "manager." My skills and interests are primarily technical and creative.
Uh, well, much like the necessary skill sets of the physician, I guess (though nowhere near in degree).
I did, however, spend a good number of my working musician years being a pretty good bandleader (adroitly herding "cats" and drawing out their talents), and -- if I may be so bold -- I was a pretty adept university "chalk talk" classroom and grad seminar teacher for a while (it was great fun). So I think I have some decent persuasive skills.
But, durably effective Leadership in the fractious arena of the healthcare space requires much more finely honed, broad and deep skills -- abilities irreducibly riding atop a solid foundation of empathic "authenticity" (points 1 and 2 above).
More on this as my study continues and my thinking clarifies. Below, from a tweet during the Forum:
Indeed. I've been having some email discussions of late with some national nursing leaders about the patient safety implications of the adversarial, dysfunctional management cultures far too prevalent in healthcare, where one speaks truth to power at one's peril.
I've worked in about seven or eight different organizational settings across the span of my white collar career. Only one of them could be considered a "safe," non-toxic culture (somewhat ironically, a hardhat clientele digital industrial diagnostics company in West Knoxville, TN, where I was a writer and our Technical Editor). The rest were burdened by differing degrees of authoritarianism, back-stabbing, and org chart climbing machinations.
It remains a problem. One all the more ironic in the "health" domain. If you work in healthcare, you know exactly to what I'm referring.
From Transforming Health Care Leadership:
More MacCoby:
We can tie some of this stuff back around to Julie Winkle Giulioni's fine book "Help Them Grow or Watch Them Go."
__
ADDITIONAL RANDOM SHOTS FROM A GREAT IHI 25 HANG
ERRATUM
The future of Obstetrics?
JUST IN: SAVE THE DATES
I will be there. Register here.
CODA
The Wall Street Journal asked yesterday for permission to use one of my HIMSS13 shots of Dr. Mostashari. Granted.

Nice. WSJ content is firewalled, but, try the link anyway.
___
More to come...
Showed this to Cheryl yesterday. We've resolved to do more of what's recommended. We've both gotten too sedentary owing to our work ("Sitting is the new Smoking").
__
LEADERSHIP
Below: a personal focus of mine at IHI 25, notwithstanding my intense interest in so many of the enticing yet too-many-to-cover tech sessions:
In healthcare (albeit -- to be fair -- as is the case with enterprise more broadly), we love our totemic cliches. "Leadership" is too often one of them.
At my last place of employ we had a group of managers (HIT, HIE, and the ED) who summarily declared themselves "Leadership."
A noun. The Department of Leadership, I guess. The Ministry of Leadership.
They spent most of their time closeted away in lengthy hush-hush, FUD angst-incubating closed-doors meetings, emerging episodically to announce their latest summary edicts.
A particularly grating pronouncement to me was an emphatic and curt declaration one day by one of them during staff meeting: "now that Leadership has decided [regarding an as-yet truly operationally unresolved issue], discussion is over."
Okee-dokee. Irony-Free Zone, much?
This increasingly autocratic attitude was one factor in my decision to retire, quite frankly.
So, "Leadership." What of it?
Google it.
143 million results. While telling, too broad.
614,000 books. OK, now we're getting somewhere. What about Amazon?
107,615 hits just in the "books" category. My fiscally-enervating Whispernet 1-click strikes yet again, twice more.
I'd noticed these in the IHI 25 Forum bookstore. Snapped cover photos in my iPhone so I could review them on Amazon (the bookstore clerk was not amused). I've downloaded and just started them. (Uh, there's that equally dubiety-inducing word "Transforming").
MacCoby's work certainly looks intriguing.
PREFACE
Who’s a Leader?Interesting. I've read and have long cited Gardener's "Changing Minds," but mostly in the context of the issues and tactical elements of persuasion, i.e., "influence" (Robert Cialdini's Influence: The Psychology of Persuasion is also compactly and effectively instructive in this regard).
THE NEED FOR LEADERS is urgent—to mobilize human intelligence and energy to grapple with historic threats such as global warming and weapons of mass destruction, and also to respond to vast opportunities to improve life on this planet. Only effective political leadership can show the way to achieve health care for all Americans, to gain energy independence through alternative nonpolluting technologies, or to fix public education so that it prepares children of every background for a demanding global economy. Only a persuasive national leader can gain support at home and abroad for policies that protect our society from its enemies. Only exceptional business and organizational leaders can provide employment and produce the goods and services essential for a strong economy. Yet despite the thousands of books and articles on the subject, we haven’t improved on classic writings about leadership. To start with, even the best recent writers on leadership stumble over the definition of a leader, and a good definition is the beginning of understanding the kinds of leaders we need and how they’ll gain followers in the context of our time.
John Gardner, a former secretary of Health and Human Services and noted leadership thinker, described very well what bureaucratic leaders do, but like a number of writers on the subject, his definition is inadequate. He defines a leader in terms of tasks: setting goals, motivating people, evaluating them. This definition doesn’t distinguish a leader from a manager or even from some leaderless teams that set their own goals and motivate each other. Other writers tell us the defining task of a leader is visioning. Certainly, many leaders have been visionaries, but lots of people with visions have no followers; some of them have ended up isolated—and even in mental hospitals.
James McGregor Burns’s brilliant treatise on leadership is full of rich historical vignettes. Burns has given us the useful distinction of transactional versus transformational leaders. By his definition, a transformational leader raises people to higher moral levels, changing them in a positive way. But this definition implies that monsters like Hitler, Stalin, and Mao weren’t transformational leaders—even though millions of people worshipped them and millions were changed by them, mostly for the worse. Even if a leader is just defined as someone who gets people to change, this wouldn’t distinguish a leader from a manager who shakes up an organization by redesigning roles and incentives. It wouldn’t even distinguish a leader from a skillful psychotherapist.
There is only one irrefutable definition of a leader, and that is someone people follow. This may seem too simple a definition for many academics, but once accepted it opens the door for plenty of hard thinking. Once we agree that anyone with followers—liberator or oppressor, transformational visionary or transactional problem solver—is a leader, then we have to answer two difficult, essential questions about leadership...
MacCoby, Michael (2007-10-04). The Leaders We Need: And What Makes Us Follow . Harvard Business Review Press. Kindle Edition.
So, persuasiveness cannot but be a core element of leadership, but what else?
I went to the day-long IHI pre-conference "Leadership Required for the New Era" for some timely and useful insights.
From their just-released White Paper:
Executive Summary
There is solid evidence that leadership engagement and focus drives improvements in health care quality and reduces patient harm. Leaders at all levels in care delivery organizations are struggling with how to focus their leadership efforts and achieve Triple Aim results for the populations they serve. Triple Aim results represent the shift from volume to value, which demands that health care leadership at every level of care delivery organizations focus on improving the experience and outcomes of care provided and reducing the cost of care for the populations they serve.
High-impact leadership is required to achieve Triple Aim results. To that end, this white paper presents three interdependent dimensions of leadership: new mental models, High-Impact Leadership Behaviors, and the IHI High-Impact Leadership Framework.
New Mental Models for Health Care Leadership
Mental models — how leaders think and view the world — are critically important because how leaders think and what they believe shapes their leadership behaviors and provides direction to focus their leadership efforts in transforming from volume-based to value-based care delivery systems. High-impact leadership requires leaders to adopt four new mental models: 1) individuals and families are partners in their care; 2) compete on value, with continuous reduction in operating cost; 3) reorganize services to align with new payment systems; and 4) everyone is an improver.
With these new mental models providing context, leaders shift the way they define success, considering new approaches and mobilizing their staff to adapt to the continually changing business environment. New mental models promote innovation.
High-Impact Leadership Behaviors
Our premise is that certain High-Impact Leadership Behaviors and practices are tightly aligned with the mental models and the leadership framework. Our list of five critical behaviors is intended to be open-ended — the starting point for health care leaders to thoughtfully examine their own leadership practices, and how they might align those behaviors with their leadership efforts and strategies to produce Triple Aim results.
- Person-centeredness: Be consistently person-centered in word and deed
- Front Line Engagement: Be a regular, authentic presence at the front line and a visible champion of improvement
- Relentless Focus: Remain focused on the vision and strategy
- Transparency: Require transparency about results, progress, aims, and defects
- Boundarilessness: Encourage and practice systems thinking and collaboration across boundaries...
Conclusion
High-impact leadership is not just for senior leaders, but is required at every level of care delivery organizations in order to deliver Triple Aim results. Value-driven, high-reliability health care sustained by improvement and innovation requires leaders at all levels to think with new mental models about the challenges and their role, practice cross-cutting High-Impact Leadership Behaviors, and focus their leadership actions through the lens of the IHI High-Impact Leadership Framework to achieve Triple Aim results for the populations they serve.
Over the past 25 years of experience and observation, IHI developed key concepts and an approach to leadership for improvement and innovation in health care. Building on this foundation, three interdependent dimensions of leadership have now been incorporated into an approach for focusing and organizing leadership efforts for leading improvement and innovation: new mental models, High-Impact Leadership Behaviors, and the IHI High-Impact Leadership Framework. The framework explicitly addresses three new areas of required leadership efforts and actions: driven by persons and community; shape desired organizational culture; and engage across traditional boundaries of health care systems.
The High-Impact Leadership Behaviors, required for leaders throughout the organization, have thus far been implemented and found effective for a group of leaders, both in and outside the health care industry. Time and experience will show if adopting new mental models and these specific behaviors will continue to magnify leaders’ effectiveness as they take on the challenges in the changing health care environment. The goal now is to provide an even larger group of leaders with the most direct path to a more person- and community-centered, effective, and agile organization. In short, there is much to be learned.Have to say, this trio of IHI presenters were quite thorough and astute. A day well spent. Much to yet ponder and assimilate.
We invite organizations to test, adapt, and share the models, behaviors, and framework offered in this white paper. As with previous frameworks, this one will benefit from learning and feedback, and IHI intends to harvest and improve on the ideas and concepts with the community of leaders. We invite feedback on what is helpful, what is missing, and what are the next steps for building strong leadership and more reliable improvement in patient experience, cost of care, and population health.
Below, one of my favorite quotes, from way back during my time in IHC healthcare QI training.
I've never really thought of myself as a "leader." And I've never had any interest in its red-headed stepchild the "manager." My skills and interests are primarily technical and creative.
Uh, well, much like the necessary skill sets of the physician, I guess (though nowhere near in degree).
I did, however, spend a good number of my working musician years being a pretty good bandleader (adroitly herding "cats" and drawing out their talents), and -- if I may be so bold -- I was a pretty adept university "chalk talk" classroom and grad seminar teacher for a while (it was great fun). So I think I have some decent persuasive skills.
But, durably effective Leadership in the fractious arena of the healthcare space requires much more finely honed, broad and deep skills -- abilities irreducibly riding atop a solid foundation of empathic "authenticity" (points 1 and 2 above).
More on this as my study continues and my thinking clarifies. Below, from a tweet during the Forum:
Indeed. I've been having some email discussions of late with some national nursing leaders about the patient safety implications of the adversarial, dysfunctional management cultures far too prevalent in healthcare, where one speaks truth to power at one's peril.
I've worked in about seven or eight different organizational settings across the span of my white collar career. Only one of them could be considered a "safe," non-toxic culture (somewhat ironically, a hardhat clientele digital industrial diagnostics company in West Knoxville, TN, where I was a writer and our Technical Editor). The rest were burdened by differing degrees of authoritarianism, back-stabbing, and org chart climbing machinations.
It remains a problem. One all the more ironic in the "health" domain. If you work in healthcare, you know exactly to what I'm referring.
From Transforming Health Care Leadership:
The Role of Culture In most medical schools, physicians are selected and trained to be autonomous craftsmen. There is little teaching about interdependence, leadership, or the importance of organization. Physicians are not trained to look at work from the viewpoint of nurses, psychologists, pharmacists, technicians, or even patients. The image of the independent decision maker that may have made the field attractive to them is reinforced by their education. Expert physicians are comfortable within a craft mode of production. Their ideal organization is their own craft shop or possibly a partnership...
No longer will patients passively wait for the health care community to tell them what to do. Their expectations are challenging the existing health care delivery systems, health care professionals, and information systems. The ability of patients to evaluate their conditions, care, and options via the Internet challenges traditional relationships, craft- and production-oriented health care systems, and their providers. Partnering and the integration of informed patients and patient advocates into the delivery system will differentiate health care organizations as they transform into the interactive health care learning environment of the future.
Physicians have run clinics or their own medical offices. Yet their education does not include courses to help them manage and improve complex health care organizations, much less lead others to do so. If physicians and nurses are to lead learning organizations, they must develop new skills and knowledge.
There is resistance to change, particularly from physicians whose social character and training support the craft mode of production. Unless the education of physicians focuses on developing the values and competencies for a learning organization, resistance will continue to impede positive change. However, we met many younger physicians with a more interactive social character who respond in a more positive way to a learning organization (see Chapter 8). Nurses are often the behind-the-scenes leaders within clinics, wards, and offices, running the business and managing patient care. They work in partnership with physicians, specialists, administrators, and other nurses. Many times they defer to the physician or manager in charge. They generally choose not to lead, even when they understand better than formal authority figures the personalities and viewpoints of physicians, nurses, and other professionals and patients. They tend to defer to the physician as the leader. They need to develop leadership competence and confidence. Leadership in learning organizations should be based on knowledge and leadership qualities, not professional affiliation. All health care workers should be respected for their distinctive competences.
Health care organizations are cultures or social systems that have purposes and are composed of people who must be motivated to achieve these purposes. These cultures differ according to their social, political, and business environments and traditions as well as their missions. They select and socialize different values in their key members. Social systems will learn and develop only when leaders align innovations with other elements of the system. Otherwise, new ideas and approaches will be limited, distorted, or totally rejected. The good news is that some of the leaders of health care organizations are becoming aware of what is required to transform their systems, and they are providing models that others can learn from, but not necessarily copy. Adaptation and testing to fit local circumstances are critical to successful implementation.
Leaders of some of the best health care organizations in the United States, Canada, United Kingdom, Sweden, and other countries strongly affirm the need to move to the learning mode of production. Elements of the learning mode are emerging in some of these organizations, but creating a learning organization requires leadership and continual development.
Policymakers should understand that solving the problems of health care delivery is not just a matter of adopting new policies and incentives, but rather of transforming a craft mode of production in a way that incorporates the best craft values into more productive, interactive learning organizations.
Leaders for health care organizations should be selected not because they are distinguished experts, but because they demonstrate strategic intelligence and understand the logic of business, quality, and leadership. They must gain the informed support of their boards, recognizing that even positive change will provoke resistance...Interesting observation about nurses. Very interesting.
More MacCoby:
Without effective leaders, health care organizations will not become learning organizations. Leaders are needed to protect the best qualities of caring and service found in the craft tradition of medicine and nursing and also build on them to establish new ways of working. With the active participation of staff, leaders are needed to continuously improve patient safety and outcomes, reduce unnecessary costs, enhance patients’experience of service, and improve population health. Above all, leaders are needed to encourage the doubters, to infuse the belief that the people can create the organization's future...
What is leadership? Leaders are people others follow. If no one follows you, you are not a leader. If you have followers, you are a leader. Leadership is a relationship. Good leadership means people willingly follow a leader who is working to further the common good, the well-being of all stakeholders. Good leaders make followers into collaborators. Leadership implies a relationship that cannot be handed off to anyone else. In contrast, management is a collection of functions. Management has to do with measurements, monitoring, HR, supply functions, and the implementation of service delivery necessary for operations. Many management functions do not require managers as teams can share these functions, even rotate them within a team, and some can be automated. Both leadership and management are necessary for the success of organizations. All managers should be leaders, and in fact, most can be developed for leadership roles. As the Institute of Medicine recommends, a continuously learning health care system requires “broad leadership.”...
Maccoby, Michael; Norman, Clifford L.; Norman, C. Jane; Margolies, Richard (2013-07-29). Transforming Health Care Leadership: A Systems Guide to Improve Patient Care, Decrease Costs, and Improve Population Health (Kindle Locations 1193-1200). Wiley. Kindle Edition.
We can tie some of this stuff back around to Julie Winkle Giulioni's fine book "Help Them Grow or Watch Them Go."
Curiosity might be the most under-the-radar and undervalued leadership competency in business today. Think about it: what could you accomplish if you practiced passionate listening— really listening with intention and a true sense of purpose to learn and understand? What ideas and possibilities could you cultivate if you honed your ability to wonder out loud with those around you?
Developing the ability to approach individuals, situations, and conversations with curiosity and even a sense of wonder can affect your own energy and enthusiasm, relationships with others, and hard business results— not to mention the quality of your career conversations.
Quality questions asked without curiosity will signal to employees that you’ve just come back from training.
Quality questions asked with the spirit of curiosity will facilitate conversations that will literally allow others to change their lives.
CLOSURE IS OVERRATED
Given this focus on asking questions, it bears repeating that you don’t have to have all the answers. Neither does the employee, for that matter. In fact, not having all the answers may actually drive more thought and energy.
According to Russian psychologist Bluma Zeigarnik (in “The Retention of Completed and Uncompleted Actions,” which appeared in Psychological Research in 1927), we remember better what’s incomplete. The problem is that this lack of closure generates an internal tension for many. The mind, uncomfortable with what has been left unfinished, continues to focus on the question or problem.
So, what does this science have to do with helping your people grow? Many managers shy away from hard questions and conversations where they might not have all the answers. If you’re one of them, you don’t have to do that any longer. Quite the opposite. Go ahead and courageously ask the challenging questions and even end the conversation with a real tough or thought-provoking one that the employee can contemplate for a while.
Don’t feel the pressure to wrap up every conversation with a bow.
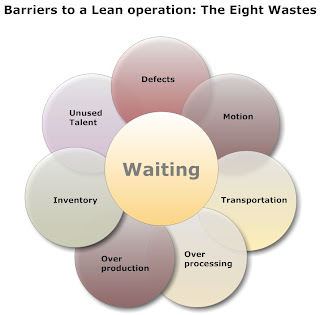
Kaye, Beverly; Winkle Giulioni, Julie (2012-09-17). Help Them Grow or Watch Them Go: Career Conversations Employees Want (BK Business) (pp. 23-24). Berrett-Koehler Publishers. Kindle Edition.Indeed. John Toussaint added an "8th waste" to the traditional "7 wastes" of Lean theory -- the waste of unused talent.
__
ADDITIONAL RANDOM SHOTS FROM A GREAT IHI 25 HANG
 |
| These kids were off-the-hook fine. Their National Anthem rendition gave me chills. |
 |
| Decent lighting, except in the various session rooms, wherein most of the presenters were literally in the dark. Learn from Health 2.0, folks, it's a live presentation, make it uniformly vibrant. |
 |
| The fabulous Dr. Mark Smith of CHCF. |
 |
| IHI CEO Maureen Bisognano during her Keynote on "flipping education and healthcare" |
 |
| Leana Wen, MD. I'm currently reading her book |
 |
| Glad to see a bit of benign neglect of healthy snacking. There was no half & half at the Health 2.0 conferences, just yucky soy and rice milk. |
 |
| The box lunches were really fine, but baked potato chips are a solution in search of a problem. Like eating lightly salted drywall flakes. |
 |
| The poster session hall was huge. A forest of great infographics. |
ERRATUM
The future of Obstetrics?
JUST IN: SAVE THE DATES
I will be there. Register here.
CODA
The Wall Street Journal asked yesterday for permission to use one of my HIMSS13 shots of Dr. Mostashari. Granted.

Nice. WSJ content is firewalled, but, try the link anyway.
___
More to come...
Subscribe to:
Comments (Atom)