A nationwide health information technology (health IT) infrastructure can offer tremendous benefits to the American public, including the prevention of medical errors, improved efficiency and health care quality, reduced costs, and increased consumer engagement. However, if health IT is not designed, developed, implemented, maintained, or used properly, it can pose risks to patients.OK. Worth your time. In particular, I find this section (below) interesting.
Section 618 of the Food and Drug Administration Safety and Innovation Act (FDASIA), Public Law 112- 144, requires that the Food and Drug Administration (FDA), in consultation with the Office of the National Coordinator for Health Information Technology (ONC) and the Federal Communications Commission (FCC) (collectively referred to for purposes of this report as “the Agencies”1), develop and post on their respective web sites “a report that contains a proposed strategy and recommendations on an appropriate, risk-based regulatory framework pertaining to health information technology, including mobile medical applications, that promotes innovation, protects patient safety, and avoids regulatory duplication.” This report fulfills the Section 618 requirement...
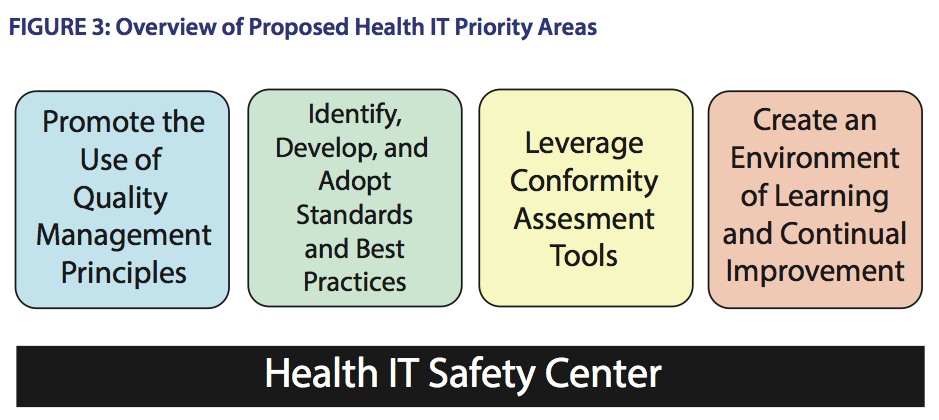
5.1 Promote the Use of Quality Management Principles
Quality management principles and processes, as part of a quality system, have been adopted and implemented by more than 1 million companies and organizations worldwide to improve quality, efficiency, safety and reliability. The selective adoption and application of existing quality management principles and processes to health IT has been advocated by the IOM, the FDASIA Workgroup, and numerous health IT stakeholders including developers, implementers and users. Some, but not all, health IT developers and healthcare facilities already adopt quality management principles.
A number of different approaches to quality management exist; however, they share certain common, underlying principles. Quality management principles help to identify, prevent, track, and monitor safety hazards and to reduce risks. They can be applied throughout the product lifecycle to design and development activities, to implementation, customization, integration, upgrades, maintenance, and operations, as well as to surveillance, reporting, risk mitigation and remediation. Importantly, quality management principles are flexible, scalable and adaptable so organizations (e.g. health IT developers, healthcare facilities, etc.) can tailor the application of these standardized processes to their individual circumstances and needs. Ultimately, quality management principles and processes provide a quality framework for companies and organizations to ensure that their products and services consistently meet their customers’ needs and requirements, that risk management principles are applied to identify, evaluate, mitigate and remediate hazards, and that overall quality is continually improved.
The judicious application of quality management principles and processes by health IT stakeholders can promote the safe design, development, implementation, customization, integration, and use of health IT while fostering an environment that promotes innovation and continual improvement. However, because health IT represents a broad spectrum of products and services, health IT developers and organizations must have flexibility to determine the necessity of individual quality elements and to tailor the development and implementation of quality management processes appropriate for their products and services.
As part of the 2014 Edition Standards and Certification Criteria final rule, ONC adopted two safety-related certification criteria for EHRs: one that focuses on the application of user-centered design to medication-related certification criteria and another that focuses on the quality management system (QMS) used during the EHR technology design. In general, the Agencies believe that additional value to health IT purchasers and users could be realized if greater transparency existed around the quality management principles that were applied in the design and development, customization and implementation, and post-deployment use of health IT.
Well, yeah. Count me in on those points. Anyone who has followed this blog since I started it knows that I come at the Health IT thing from an old-school QI perspective, given my long activist affiliation with ASQ. See my opening 2010 post Opportunity for collaboration? ASQ and the RECs (the one that immediately got me in "exceeding your scope" soap opera uproar trouble with my overcaffeinated Executive Director).
"As part of the 2014 Edition Standards and Certification Criteria final rule, ONC adopted two safety-related certification criteria for EHRs: one that focuses on the application of user-centered design to medication-related certification criteria and another that focuses on the quality management system (QMS) used during the EHR technology design."Well, with respect to the latter assertion, inexorably The Power of Photoshop Compelled me.
Yes, it's optional. §170.314(g)(4):
(i) If a single QMS was used for applicable capabilities, it would only need to be identified once.Pretty weak. Why they even bothered escapes me. PR fig-leafery?
(ii) If different QMS were applied to specific capabilities, each QMS applied would need to be identified. This would include the application of a QMS to some capabilities and none to others.
(iii) If no QMS was applied to all applicable capabilities such a response is acceptable to satisfy this certification criterion. [emphasis mine]
___
More to come...


No comments:
Post a Comment