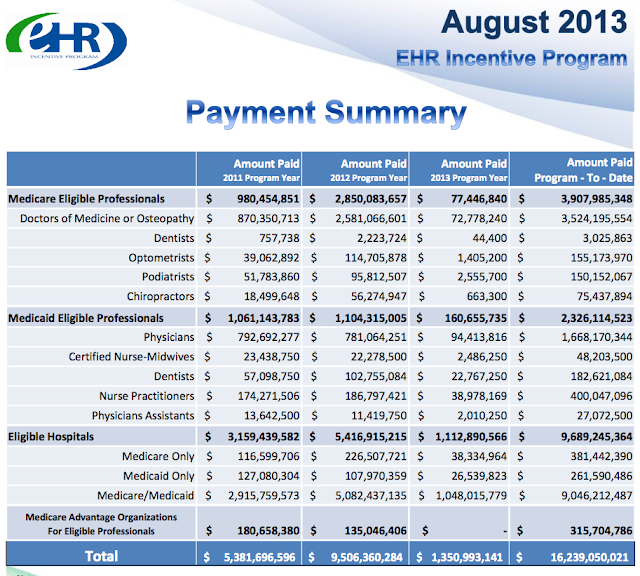
Incentive payments up from $15.9 billion to $16.2 billion, not much of a relative increase,m as was the case last time. Unsurprising this time of year for those on calendar year MU.
Equally interesting are the merged ONC+CMS data tabluting attestations by vendor and product.
Presenting here only to top 20 as ranked. Epic continues to rule. But, eClinicalWorks has done a great job, coming in 3rd, amid much larger players. And, the free Practice Fusion ranks 10th.
Below, the data dictionary for the ONC-CMS aggregated data.
Lots of ways to stratify/"peel back the onion." Geographically granular to the state level, but many other perspectives to be had as well. Had I SAS or Stata install I'd probably have already sliced 'n diced these data 16 ways to Sunday, just out of empirical curiosity. Excel pivot tables are OK, but clunky and slow in comparison.
Top Attestors by specialty below.
Note: "PEP" here in my tally means "Priority Eligible Provider," i.e., those who can engage the RECs for ONC-subsidized technical assistance. Also often referred to as "PPCPs."
__
Moving on to the 2014 CEHRT data. A lot of concern has been expressed regarding the extreme paucity of 2014 ONC certifications to date. e.g.,
A mere 20 vendors certifying only 27 complete ambulatory products at this point. There are 1,767 ONC 2011 MU complete systems certified to date. (In fairness, that's an overcount, given that many vendors certify successive releases of the same product. I'd need to run a "PROC SORT; by EHR Product NODUPES;" on the data in SAS for a quick, clean boiled-down complete tally. Still, there are hundreds.)
UPDATE: a quick screen scrap and Excel dump shows the Cert redundancies and overcount problem (2011 cert data), given the CHPL certs for every major and minor version releases.
(Note: the material difference between eCW "9" and"9.0" escapes me. It's just what I found there.)
It's even more sparse on the inpatient side. Below, screen-snipped directly from ONC CHPL:
Only eight vendors certifying complete inpatient EHRs.
What, me worry? Stage 2 Year 1 has already commenced for certain Eligibles operating on the federal fiscal year.
The recently added, weasely "Combination of 2011 and 2014 Edition" is pretty vague.
You have selected the ‘Combination of 2011 and 2014 Edition’ EHR certification criteria for attestation. You can use EHR technology that is certified to 2011 edition certification criteria AND/OR the equivalent 2014 edition certification criteria to generate CMS EHR Certification ID that is submitted to CMS as part of attesting to meaningful use of certified EHR technology.__
OCT 23 UPDATE:
Stage 2 proves challenging for vendorsMaybe we should put CGI Federal on it. They don't seem to have been real busy of late.
'Surprised by the complexities' of the new requirements, some EHR makers have 'certification fatigue'
October 23, 2013, Diana Manos, Anthony Brino
“It has been a slow start," said Alisa Ray, executive director and CEO of the Certification Commission for Health Information Technology, of EHR vendors' readiness for Stage 2 meaningful use. "They’re working hard. They’re struggling a little bit."
That stands to reason, considering that, when comparing Stage 1 to Stage 2 certification, technology developers are "navigating a higher bar and increased complexity," she said.
As the end of 2013 closes in, most federal certification bodies are noticing an uptick in the number of vendors who are applying to become certified under the 2014 criteria — the same criteria that will be required for the EHR products providers must use to attest to meaningful use Stage 2.
But not all of them are finding the process to be a cakewalk. Ray said there are three areas of Stage 2 that are proving the most challenging for certification: clinical quality measures, interoperability, and automated measure calculation for reporting metrics.
Automated measure calculation “requires almost a whole day of testing,” she said. “There are just a lot fewer products than were there with the Stage 1 or 2011 criteria.”...
And without naming names, Ray said that “almost everyone has struggled and been surprised by the complexities,” and a number of them have had to go through several certification trials, after not meeting certain criteria. “There are companies that have been testing every year since 2006 with the CCHIT programs; it’s not like they’re novices. And when they get into it, there’s a new wrinkle or something they may not have anticipated or configured correctly.”
It’s important to keep in mind, she said, that it’s a combination of the criteria and ONC’s testing methods that really defines “the exact nuances of what the product needs to be able to do.”...
But wait! There's more! From THCB:
...According to Modern Healthcare, natural selection may already be taking place in the EHR environment as Meaningful Use 2014 and Stage 2 introduce more exacting requirements. The magazine’s review of federal records shows a massive drop in the number of health IT systems being tested for Stage 1 2014 and Stage 2 certification. While around 1,000 EHR technologies were certified for 2011 Stage 1 requirements, as of last week only 79 systems were certified for 2014 standards. Almost all companies are scrambling. Some will get certified in time. Many more won’t.__
“This is just the beginning of the shakeout … there is an asset bubble in electronic health records and health IT,” said Dr. David Brailer, founder and CEO of Health Evolution Partners and former head of the Office of the National Coordinator for Health Information Technology.
“The data suggests that it is likely we’ll see a sizable reduction in the number of EHR vendors listed for 2014 edition certification,” predicted Steven Posnack, director of federal policy, and Dustin Charles, a public health analyst, on the ONC’s September 13 blog post...
UPDATE: Nice, from Jim Tate, Healthcare IT News
What not to do in a meaningful use auditIndeed.
6 things to avoid if you want to protect those incentive payments
October 21, 2013
- Having no one in charge. Assign a committee to be responsible for the audit process and requests for documentation. When things go wrong there will be plenty of people to blame.
- Having insufficient documentation. Just assume you can always go back and recreate reports that you can't find. All that data is in there somewhere, I'm sure we can find it if we need to.
- Ignoring requirements. We are not really sure what is this "syndromic surveillance submission" business. We only have to do one test? Let's just say "yes" and move on.
- Having an undocumented MU strategy. What was the reasoning behind those core measures that were excluded and menu measures that were not chosen? Who was that staff member that made the decisions?
- Blaming the EHR vendor. This entire mess was created by our vendor. It is their job to make sure there are no problems. They should be responsible and make this go away.
- Failing to perform a Security Risk Assessment. I'm pretty sure we did one of these a few years back and it was OK. Probably still good now.
More on the topic:
Meaningful Use attesters: Beware the False Claims ActI'd like to know the extent of MU audit failures triggering Incentive paybacks.
October 17, 2013 By Marla Durben Hirsch
We know what the drill is when providers attesting to Meaningful Use are later audited to see if they really were entitled to their incentive payments. If auditor Figliozzi and Company determines that the provider did not meet the attestation requirements, the provider will receive a letter directing it to return the "overpayment" to the government within 30 days to avoid having to also pay interest. If the debt still is not paid within 60 days, the debt is referred to the U.S. Department of the Treasury for possible offset. A number of people who have dealt with these audits have shared the details of the letters used; the Centers for Medicare & Medicaid Services even provides some information on its website...
...CMS does state in the regulations that it believes that attestations are subject to the False Claims Act. This issue is particularly sticky because Meaningful Use is an "all or nothing" deal; if one component of the attestation is faulty, the provider must return all of the money. No partial credit...
The False Claims Act is not to be taken lightly. Penalties range from $5,500 to $11,000 per claim, and are subject to treble damages. The U.S. Department of Health & Human Services has recovered millions of dollars from providers by using the False Claims Act. Moreover, it allows individuals to become whistleblowers and bring their own action against a provider, receiving a percentage of the amounts recouped. This leave providers particularly vulnerable.
We already know that improper billing by EHR users is on the government's radar. I would not be surprised if the government also starts using the False Claims Act to go after improper attestation...
31 USC § 3729 - False claims"knowingly presents or causes to be presented..."
(a) Liability for Certain Acts.—
(1) In general.— Subject to paragraph (2), any person who—
(A) knowingly presents, or causes to be presented, a false or fraudulent claim for payment or approval;
(B) knowingly makes, uses, or causes to be made or used, a false record or statement material to a false or fraudulent claim;
(C) conspires to commit a violation of subparagraph (A), (B), (D), (E), (F), or (G);
(D) has possession, custody, or control of property or money used, or to be used, by the Government and knowingly delivers, or causes to be delivered, less than all of that money or property;
(E) is authorized to make or deliver a document certifying receipt of property used, or to be used, by the Government and, intending to defraud the Government, makes or delivers the receipt without completely knowing that the information on the receipt is true;
(F) knowingly buys, or receives as a pledge of an obligation or debt, public property from an officer or employee of the Government, or a member of the Armed Forces, who lawfully may not sell or pledge property; or
(G) knowingly makes, uses, or causes to be made or used, a false record or statement material to an obligation to pay or transmit money or property to the Government, or knowingly conceals or knowingly and improperly avoids or decreases an obligation to pay or transmit money or property to the Government,
is liable to the United States Government for a civil penalty of not less than $5,000 and not more than $10,000, as adjusted by the Federal Civil Penalties Inflation Adjustment Act of 1990 (28 U.S.C. 2461 note; Public Law 104–410 [1] ), plus 3 times the amount of damages which the Government sustains because of the act of that person.
__
NYEC 2013 CONFERENCE NEXT MONTH
The Digital Health Conference brings together a diverse group of professionals for two days of lively intellectual exchange.They've granted my press pass. I'm registered and booked.
Healthcare providers, IT innovators, health leadership, start-ups, hospital officials, group practice managers, investors, and entrepreneurs will gather to hear insights, ideas, and analysis from leaders in the health IT community.
Engage with thought-provoking lectures, interactive panels, emerging IT tools, technological exhibits, networking and discussion.
The event will be held at the Hilton New York, in the heart of Manhattan, and will showcase practical, innovative, and inspiring advancements in health information technology.
__
INTERESTING TIDBIT ON THE HEALTHCARE.GOV MESS
Written Testimony of Cheryl Campbell, Senior Vice President CGI Federal Inc.
Prepared for
The House Committee on Energy and Commerce Subcommittee on Health
September 10, 2013
Chairman Pitts, Congressman Pallone, Members of the Committee, thank you very much for the opportunity to appear before you today. My name is Cheryl Campbell and I am a Senior Vice President at CGI Federal Inc. (CGI Federal), a company that has provided information technology (IT) and business process services to the federal government for more than 36 years. In my role, I lead CGI Federal’s Health and Compliance Programs Business Unit, including responsibility for all of its projects at the Department of Health and Human Services (HHS) and several other federal agencies. It is my pleasure to appear today before you at this hearing to discuss CGI Federal’s role as the contractor designing and developing the complex, IT application known as the Federally-Facilitated Marketplace (FFM), formerly known as the Federal-Facilitated Exchange. The FFM application, one of several components being developed in a multi-stakeholder environment, will allow citizens, health insurance issuers, the Centers for Medicare and Medicaid Services (CMS), and many States to participate in the marketplace for affordable health insurance mandated by the Patient Protection and Affordable Care Act (PPACA).
On September 30, 2011, CMS conducted a competitive procurement and selected CGI Federal to design and develop the FFM. CMS issued CGI Federal a task order for this work under CGI Federal’s Enterprise Systems Development, Indefinite-Delivery, Indefinite-Quantity type contract. Currently, the task order includes: a 29-month Base Period for design, development, and implementation; one (1) 6-month and two (2) one-year Option Periods for operations and maintenance; and a 6-month Transition Out Period.
The task order directs CGI Federal to design and develop a FFM that will perform the functions and business processes that CMS has identified in regulations and guidance issued pursuant to the PPACA. At the time of task order award, most of these regulations and guidance were still being finalized and the associated system requirements defined fully. For that reason, the FFM task order was issued as a cost-reimbursement type task order and the project’s original scope was defined broadly with deliverable dates to be determined by CMS. During the course of performance, CMS has modified the task order on several occasions, generally in response to more detailed requirements regarding system functionality as regulations and policy were better defined.
Generally, CGI Federal’s scope of work includes the following three (3) work streams:
1) Architecting and developing a FFM that may be used by any State that opts out of building and operating its own marketplace;
2) Designing an IT solution that is adaptable and modular to accommodate the implementation of additional functional requirements and services; and
3) Participating in a collaborative environment and relationship in support of the coordination between CMS and its primary partners.
When open enrollment begins on October 1, 2013, the FFM will have three (3) key functions to assist citizens in comparing, selecting, and enrolling in qualified health plans in States that have chosen not to build their own marketplace. These three (3) key operational functions include:
1) Eligibility & Enrollment. The FFM will serve as the “front door” for consumers to fill out an online health insurance application, determine their eligibility for health insurance, and enroll in a qualified health plan. Among other things, the FFM will interface with a Data Services Hub being developed by a contractor under another contract to access income, citizenship, and the information necessary to determine an individual’s eligibility for health insurance, and whether that individual also is eligible for subsidies or credits. The FFM also will allow citizens to view, compare, select, and enroll in health plans available through the exchange.
2) Plan Management. The FFM will serve as the entry point for health insurers to submit plans for CMS certification as qualified health plans. CMS will use the FFM to acquire, certify, and manage issuers offering qualified health plans through the FFM. CMS also will coordinate plan management activities with States, including monitoring and oversight, account management, and recertification. Health insurers began submitting their plans to the system in April 2013.
3) Financial Management. The FFM will allow CMS to manage financial transactions with issuers, including calculating reinsurance payments, risk adjustments and corridors, and premium processing.
Under CGI Federal’s task order, CMS is responsible for establishing the business processes and general requirements for the FFM system and CGI is tasked with designing and developing an IT architecture to achieve these requirements. The business processes and general requirements come from the PPACA and regulations, policy, and guidance issued by CMS, CMS’ requirements contractor, and other Federal agencies and are influenced by the diverse approaches individual States have adopted to implement the law. To that end, the IT solution has been structured to support CMS as it provides three (3) implementation model options to the States. In the most basic terms, these three (3) options are:
1) Federally Facilitated Marketplace – HHS operates the marketplace for a State;
2) State Partnership Marketplace – A State operates plan management or customer support or both and HHS operates the remainder of the marketplace for that State; and
3) State-Based Marketplace – A State operates the entire marketplace, but has the option to use HHS Support for certain activities.
To date, the FFM implementation has achieved all of its key milestones from the initial Architecture Review in October 2011 to Project Baseline Review in March 2012 and, most recently, the Operational Readiness Review in September 2013. Additionally, in April 2013, health insurers began submitting their plans to the system for review by CMS. Starting in August 2013, consumers were able to go into the system and register their accounts.
At this time, CGI Federal is confident that it will deliver the functionality that CMS has directed to enable qualified individuals to begin enrolling in coverage when the initial enrollment period begins on October 1, 2013.
Moving forward, CGI Federal also is confident in its ability to deliver successfully on its task order and remains committed to the success of the FFM as a key mechanism for providing health care coverage by the statutory deadline of January 1, 2014. I appreciate the opportunity to appear before you today and would be pleased to answer any questions that you may have."At this time, CGI Federal is confident that it will deliver the functionality that CMS has directed to enable qualified individuals to begin enrolling in coverage when the initial enrollment period begins on October 1, 2013."
__
Pass the popcorn.
Scroll back down through my prior post. See also, from Kaiser Health News:
Defending Health Exchange's Rollout Puts Sebelius In Hot Seat
JUST IN...
The White House is sending in teams of experts to fix badly broken Healthcare.gov. The project has 55 contractors. Sending in SWAT teams of politically connected individuals who know nothing about the project but want it fixed NOW is a recipe for more disaster....
Read the entire piece. Excellent.
___
More to come...











No comments:
Post a Comment